Sleep apnea is a sleep disorder in which breathing repeatedly stops and starts. There are three different types of sleep apnea which have similar symptoms, making it difficult to determine which type a patient may have. Obstructive sleep apnea (OSA) is the most common form that occurs when the throat muscles relax and cause a narrowing or collapse of the pharyngeal airway. This causes symptoms of loud snoring, gasping for air during sleep, dry mouth, morning headache, daytime sleepiness, and insomnia. Central sleep apnea occurs when the brain does not send proper signals to the muscles that control breathing. The third form is called complex sleep apnea which is a combination of both obstructive sleep apnea and central sleep apnea.
OSA occurs when the muscles that support the soft palate, uvula, tonsils, and side walls of the throat relax. These disruptions to breathing lead to intermittent blood gas disturbances (hypercapnia and hypoxemia) and surges of sympathetic activation. When this occurs, the brain senses the inability to breathe and briefly awakens the patient from sleep. This can happen anywhere from five to thirty times an hour, making it difficult to reach deep, restful phases of sleep.
Although anyone can develop OSA, there are factors that can put an individual at an increased risk of developing this condition. Excess weight or obesity, hypertension, nasal congestion, smoking, and diabetes can put an individual at an increased risk. Genetics can also play a role if a person inherits a naturally narrow airway.
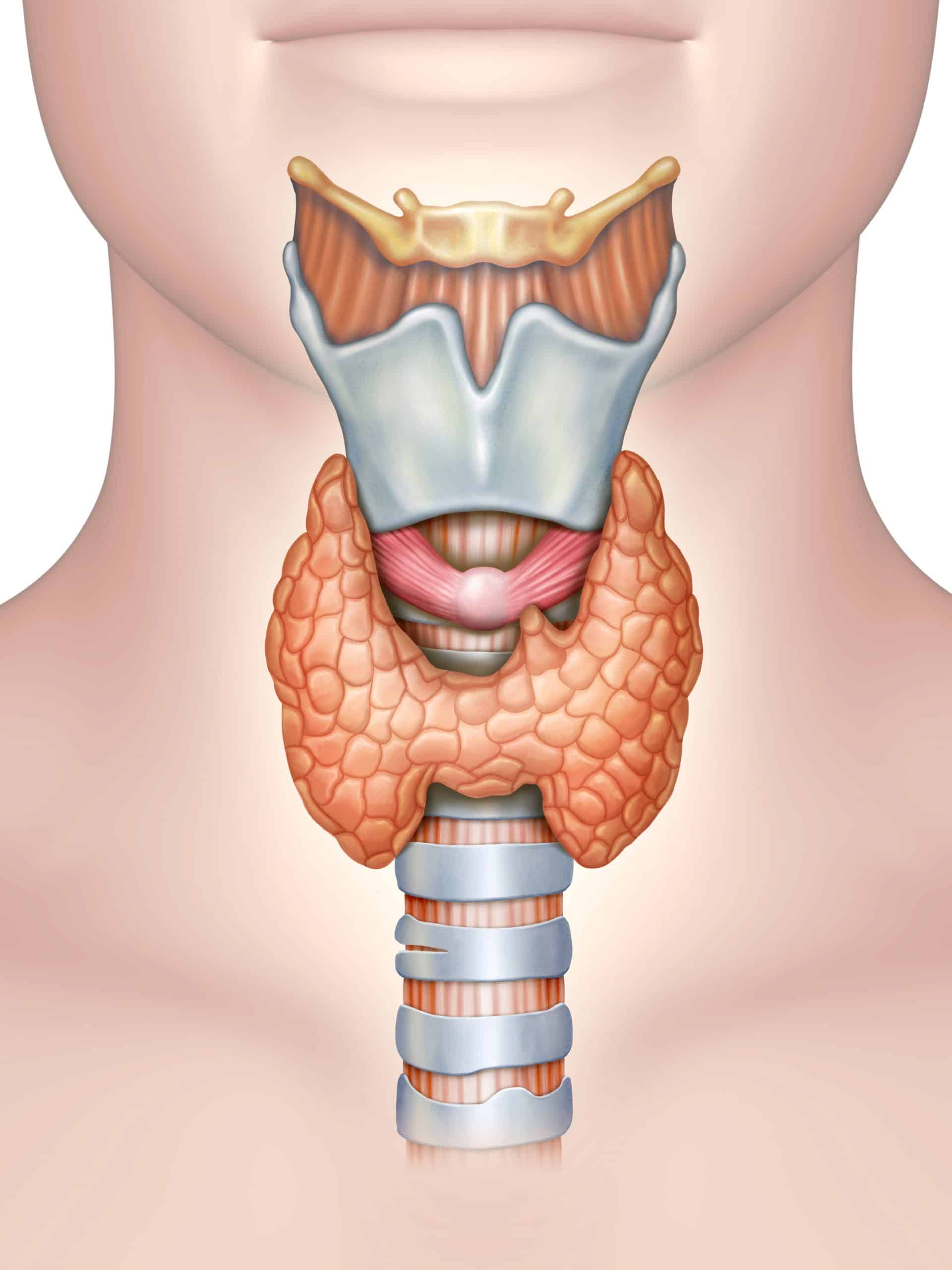
The upper airway is composed of numerous muscles and soft tissue but lacks rigid or bony support. Most notably, it contains a collapsible portion that extends from the hard palate to the larynx. Although the ability of the upper airway to change shape and momentarily close is essential for speech and swallowing during wakefulness, this feature also provides the opportunity for collapse at inopportune times such as during sleep. Therefore, from an anatomical perspective, a narrow airway is generally more prone to collapse than a larger one.
One mechanism believed to be important in the pathogenesis of OSA relates to the interaction between pharyngeal anatomy and a diminished ability of the upper airway dilator muscles to maintain a clear and definite airway during sleep. Ventilatory control plays a big role in the dilator muscles staying clear. Obstructive events tend to occur during periods of low respiratory drive. Decreased lung volume, or Cold Lung in TCM, causes a decrease in upper airway responsiveness which leads to the narrowing and collapse of the throat. A study done on overweight OSA patients showed that the pharyngeal airway decreases as lung volume decreases. This cycle of hyper and hypo ventilation can occur throughout the whole night.